Calf Augmentation: A Single Institution Review of Over 200 Cases
Article Published In: The American Journal of Cosmetic Surgery Vol. 30, No. 2, 2013
Paul N. Chugay, MD; Nikolas V. Chugay, DO
Introduction: Over the past several decades, there has been increased interest in creating a fuller-appearing and more well-defined calf region.
The primary method for augmentation is the use of a semirigid silicone prosthesis as it produces reliable results and an aesthetically pleasing calf contour.
Materials and Methods: A retrospective review of patient charts was performed to identify patients who had undergone calf augmentation from 2007 through 2011. The charts were reviewed for patient satisfaction, the size of the implant, and observed complications.
Results: A total of 202 calf augmentations were performed over the 5 years studied. The overall satisfaction rate was 92.1% (186/202). Patients who were unsatisfied with the procedure were primarily dissatisfied with the amount of augmentation achieved or by hypertrophic scarring.
Conclusions: Calf augmentation is a procedure that can nicely enhance the physique in a reliable fashion. The overall satisfaction rate is excellent as long as care is taken to ensure that the right implant is chosen to meet the patient’s expectations, that meticulous attention is paid to dissection of the pocket to minimize implant migration, and that a layered closure is used to minimize hypertrophic scarring.
Over the past several decades there has been increased interest in creating a fuller-appearing and more well-defined calf region. Men and women alike wish to have a more muscular and toned physique. Despite vigorous exercise and bodybuilding, however, some people are unable to attain the definition that they desire. Many patients who present for consultation want to look good in shorts and skirts but believe they are unable to do so because they have a hypoplastic calf. To that end, calf implants of various shapes and sizes have been created to increase volume in the calf. In addition to calf implants, there has been increasing interest in the use of fat to augment the calf to avoid foreign body placement. However, the primary method for augmentation is still the use of a semirigid silicone prosthesis as it produces reliable results with an aesthetically pleasing calf contour. With this in mind, we sought to evaluate the procedure and review the associated risks and complications seen in our body implants practice from 2007 through 2011.
Methods
A retrospective review of patient charts was performed to identify patients who had undergone calf augmentation from 2007 through 2011. All patients underwent calf augmentation with silicone implants. The charts were reviewed for patient satisfaction, the size of the implant, and observed complications. Satisfaction was assessed at the 6-month postoperative visit by asking the patient. Are you happy with the results of your surgery and if not why? All patients were assessed at 1 day, 1 week, 1 month, 6 months, and 1 year after surgery. Long-term follow-up beyond 1 year is not routinely requested of our patient population, so the information is not available for this study.
Relevant Anatomy
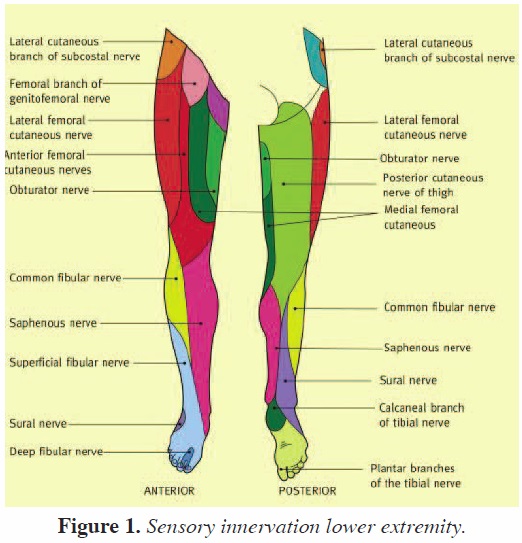
As a result of anatomic studies and operative dissections, the anatomy of the calf region is well understood. The calf is made up of 2 muscle groups: the gastrocnemius and the soleus. The gastrocnemius has 2 heads and lies superficial to the deeper soleus muscle. The 2 heads of the gastrocnemius are connected to the condyles of the femur by strong, at tendons. The medial and larger head originates from a depression at the upper and back part of the medial condyle and from the adjacent part of the femur. The lateral head arises from an impression on the side of the lateral condyle and from the posterior surface of the femur immediately above the lateral part of the condyle.
*INDIVIDUAL RESULTS WILL VARY. IMAGES DO NOT CONSTITUTE A PROMISE OR REPRESENTATION OF ANY PARTICULAR OUTCOME OR EXPERIENCE.
Once a sufficient pocket is dissected, the pocket is irrigated with a solution containing normal saline, betadine, Ancef, and gentamicin. Next, 15 mL of 0.5% marcaine is injected into the pocket for postoperative analgesia. A lozenge-shaped implant is then placed into the pocket, making sure to attain symmetry (Figure 4).
Once the implant has been placed, symmetry is assessed. At this point, closure is begun. The fascia is reapproximated with 2-0 Monocryl suture in an interrupted fashion. The deep dermis is reapproximated with 3-0 Monocryl suture in buried fashion. The skin is closed in subcuticular fashion with 4-0 Vicryl suture or interrupted 4-0 silk sutures (based on the surgeon’s preference). The same procedure is mirrored on the contralateral side. The legs are wrapped with Coban, and the patient is then taken to the postanesthesia care unit.
Postoperative Care
Postoperatively, the patient may begin ambulating starting on the evening of the procedure and may shower on postoperative day 1, making sure to keep dressings clean and to dry the Robbins tape with a hairdryer on a low heat setting. Patients are then allowed to begin light activity at week 2 and full activity at weeks 4-6. Patients are asked to wear compression stockings with a grading of 20-30 mmHg to prevent dead space, thereby helping to reduce the risk of seroma formation.
Results *
*INDIVIDUAL RESULTS WILL VARY. THESE RESULTS DO NOT CONSTITUTE A PROMISE OR REPRESENTATION OF ANY PARTICULAR OUTCOME OR EXPERIENCE.
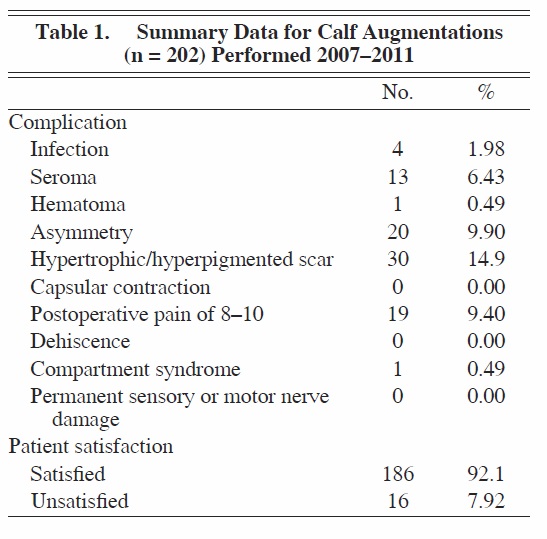
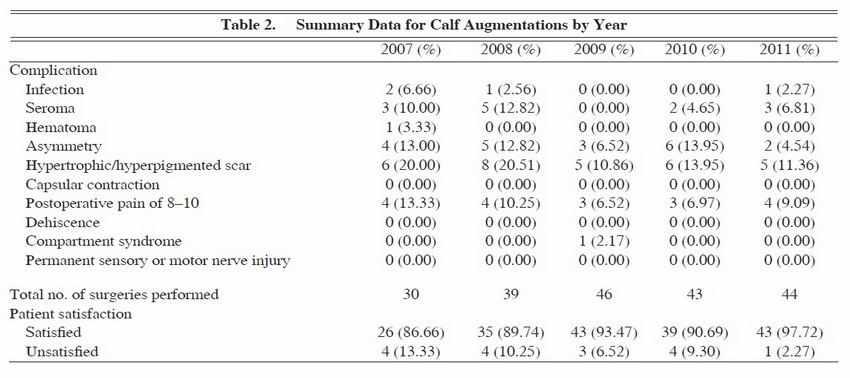
A total of 202 calf augmentations were performed over the 5 years studied (see Tables 1 and 2). The overall satisfaction rate was 92.1% (186/202). Patients who were unsatisfied with the procedure were primarily dissatisfied with the amount of augmentation achieved or by hypertrophic scarring noted in the postoperative period. The most frequently observed complication was hypertrophic/hyperpigmented scarring, which was noted in 30 of 202 patients (14.9%).
*
*INDIVIDUAL RESULTS WILL VARY. THESE RESULTS DO NOT CONSTITUTE A PROMISE OR REPRESENTATION OF ANY PARTICULAR OUTCOME OR EXPERIENCE.
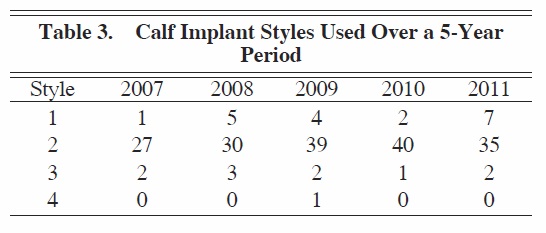
Asymmetry was noted in 20 of 202 patients (9.90%), and seromas were noted in 13 of 202 patients (6.43%). Only one hematoma was noted (0.49%). Pain was relatively well controlled in our cohort of patients, with only 19 patients (9.40%) complaining of pain rated as 8-10 on a 10-point scale. Infection was rare and was noted in only 4 of 202 patients (1.98%). No cases of capsular contracture or dehiscence were noted by the 1-year mark, and there were no cases of long-term motor or sensory nerve damage. Only one case of compartment syndrome occurred, and that was in a patient who received an implant that was too large in the medial calf region. A review of the records revealed that our preference was to use style 2 calf implants (AART, Reno, Nev) (Table 3; Figures 5 through 7).
*

*INDIVIDUAL RESULTS WILL VARY. IMAGES DO NOT CONSTITUTE A PROMISE OR REPRESENTATION OF ANY PARTICULAR OUTCOME OR EXPERIENCE.
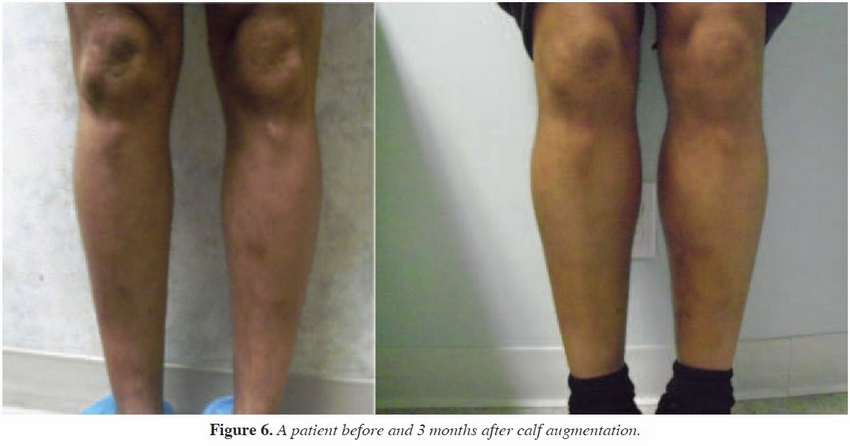
*INDIVIDUAL RESULTS WILL VARY. IMAGES DO NOT CONSTITUTE A PROMISE OR REPRESENTATION OF ANY PARTICULAR OUTCOME OR EXPERIENCE.
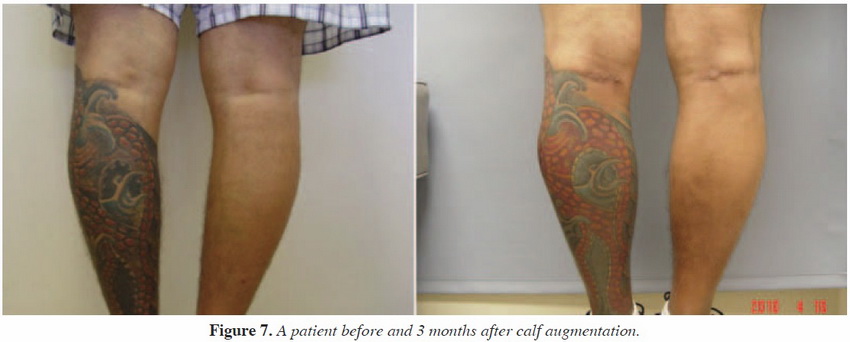
*INDIVIDUAL RESULTS WILL VARY. IMAGES DO NOT CONSTITUTE A PROMISE OR REPRESENTATION OF ANY PARTICULAR OUTCOME OR EXPERIENCE.
Discussion
Over the years, multiple physicians and mathematicians have tried to define beauty and what constitutes a beautiful human form. It was Howard2 who first described the ideal length proportions of the calves, basing his findings on the drawings of Leonardo da Vinci. Howard defined the golden ratio of calf aesthetics thus: the distance between the ankle and the lower border of the gastrocnemius muscle should equal the distance between the knee and the most prominent point on the medial curvature of the gastrocnemius
muscle. The entire length of the gastrocnemius should be 1.6 times the former value. Based on his 12 years of experience with calf augmentation, Szalay3 also helped to define the aesthetics of the calf by determining that the attractive range for female calf circumference is between 33 and 36 cm. Values outside this range are considered aesthetically unattractive.
Calf augmentation was originally designed to fill defects left after oncologic surgery, after trauma or infection, or because of genetic abnormalities. Causes of unilateral or bilateral calf deformities and include, but are not limited to, the following: congenital hypoplasia due to agenesis of a calf muscle or adipose tissue reduction; sequelae of clubfoot (talipes equinovarus), cerebral palsy, polio, or spina bifida; poliomyelitis or osteomyelitis; fracture of the femur; and burn contracture.
After it appeared in the reconstructive setting, calf augmentation evolved into a cosmetic procedure to help patients with no preexisting deformity attain a more shapely appearance. Glitzenstein2 and Carlsen4 first discussed calf augmentation in 1979, and since then, many authors have discussed their experience with the procedure.3,5–11
Some authors have noted that calf prostheses have several disadvantages: they cannot adequately correct ankle deformities, and there is a risk of displacement, capsular contracture, or problems with extrusion. Although we agree that calf augmentation does not correct ankle deformities, which may best be addressed with fat grafting, we believe the risks of displacement, capsular contracture, and extrusion can be well controlled with meticulous technique and proper postoperative care.
The only major complication noted in this study was a case of suspected compartment syndrome. Four days postoperatively, the patient presented with severe pain in his calf and minor serosanguineous drainage. On physical examination, the skin over the medial calf and dorsal aspect of the foot was found to have a dusky appearance. The patient had an intact dorsalis pedis pulse and motor was grossly intact. Serosanguineous drainage was noted from the calf incision when the leg was compressed. There was pain on palpation over the entire the calf. The patient was promptly sent to the local hospital for admission and urgent ultrasound to evaluate for any collections or deep vein thrombosis. No collections or deep vein thrombosis were noted. The patient was admitted to the hospital for neurovascular checks every hour to follow progression of the suspected compartment syndrome. The patient did not have full-blown compartment syndrome, likely because of the decrease in pressure resulting from open drainage of serous ß uid. Three days later, the patient was discharged with no pain, a strongly palpable dorsalis pedis pulse, and good motor function in the lower extremity. He had no further sequelae.
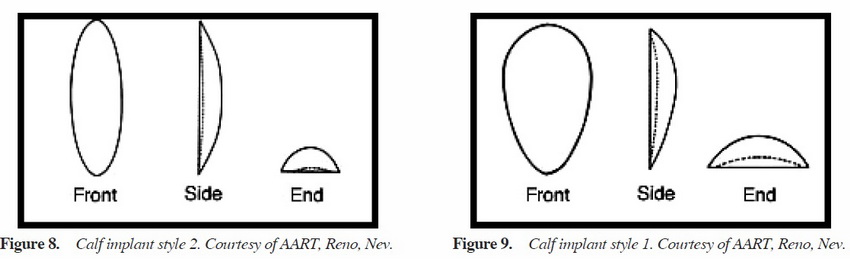
When determining the type of implant to use, we base the determination largely on the desires of the patient. However, as mentioned previously, we also take into account the length from popliteal fossa to the insertion of Achilles tendon to better define the length that can be accommodated. If the patient merely wishes to have more definition in the calf, then we will use style 2 implants in most cases. With the style 2 calf implant, there is a greater enhancement of the medial calf muscle (Figure 8). If, however, the patient wishes to have more overall volume to the calf region and is looking for a more blocklike appearance, then we favor style 1 implants (Figure 9). With the style 1 implant, there is a greater enhancement of the entire calf region, which in our practice is best suited for patients who already have a great deal of muscle volume (eg, bodybuilders) and just want an overall increase in volume. Style 3 implants are rarely used, only for lateral head augmentation. The style 4 implant is a custom implant made for a patient with significant deformity to the calf necessitating significant volume addition to the area that cannot be well addressed with existing calf implants. Each of the different style of implants has a range of sizes to fit each patient’s need. Regardless of the implant chosen, the position of the implant is always in the subfascial plane, which minimizes dissection around key neurovascular structures. With experience, a surgeon will be better able to determine the best implant for each patient.
Conclusion
Calf augmentation with silicone implants is a procedure that can nicely enhance the physique in a reliable fashion. The overall satisfaction rate is excellent, as long as care is taken to ensure that the right implant is chosen to meet the patients expectations, that meticulous attention is paid to dissection of the pocket to minimize implant migration, and that a layered closure is used to minimize hypertrophic scarring. Further studies are needed to evaluate the long-term complications and satisfaction of these patients beyond the 1-year mark.

