Weight Loss Tongue Patch: An Alternative Nonsurgical Method to Aid in Weight Loss in Obese Patients
Article Published In: The American Journal of Cosmetic Surgery Vol. 31, No. 1, 2014
Paul N. Chugay, MD; Nikolas V. Chugay, DO
Click on the PDF link above to see a copy of the article written on the tongue patch which was published in the American Journal of Cosmetic Surgery in 2014
Introduction: Despite efforts on the part of patients, some are not able to achieve significant weight loss because of poor compliance with balanced diets and exercise programs. The tongue patch is a means of ensuring that the patient abides by a strict low-calorie diet plan to achieve maximal weight loss while engaging in a moderate exercise regimen.
Materials and Methods: A retrospective chart review was performed on patients who underwent the tongue patch procedure from 2009 to 2013. All patients had a piece of Marlexmesh affixed to the tongue using prolene sutures. At the 30-day mark, each patient’s weight was recorded. Data were then tabulated. Complications were also identified from the patient charts and analyzed.
Results: A total of 81 patients received the tongue patch. Mean weight loss was 16.0 lb (range = 0-37 lb). The total weight lost by all participants was 1104.5 lb. The average starting body mass index was 32.4 (range = 24.3-45.3) and the average change in body mass index was 2.9 (range = 0-5.1). No serious complications were noted.*
Conclusions: While maintaining a strict low-calorie diet plan and adhering to a regular exercise regimen, patients using a tongue patch can achieve significant weight loss over a 30- day period with relatively minimal procedural risk.
In the 21st century, great concerns persist regarding the obesity epidemic in the United States. Based on statistics from 1999 to 2002, an estimated 30% of persons in the United States met the criteria for obesity, a statistic that is mirrored in many industrialized countries around the world. Severe obesity is known to carry higher mortality and morbidity. The health consequences of obesity include heart disease, diabetes, hypertension, hyperlipidemia, osteoarthritis, and sleep apnea. Weight loss of even 5-10% has been associated with a marked reduction in the risk of these chronic diseases and the incidence of diabetes.
Physicians are constantly working to improve the quality of life and health of their patients by advocating maintenance of a healthy weight, but unfortunately, an admonition about the need to lose weight is not enough for most patients. Occasionally, physicians need to use other tools, such as low-calorie diets, medications, and surgical procedures to help patients achieve lower healthier weights.
As a general statement, the National Institutes of Health (Nlli) says obesity should be treated with one or more of the following strategies: a diet low in calories, increased physical activity, behavior therapy, prescription medications, and/or weight loss surgery.
Over the years, physicians have developed various diet plans to help patients lose weight. The Nlli has further classified the types of low-calorie diets that are currently available to help patients achieve weight loss goals. A low-calorie diet is between 1000 and 1600 kcal/day; it consists of regular foods but may include meal replacements. A very-low-calorie diet (VLCD), on the other hand, provides up to 800 kcal/day. VLCDs use commercial formulas, usually liquid shakes, to replace all your regular meals. A VLCD is meant for short-term, rapid weight loss and is often used to jump-start a long-term obesity treatment program. Despite the significant weight loss that can be achieved with a VLCD, the Nlli warns that weight loss can only be maintained if the patient adopts a healthy, long-term eating plan and good physical activity habits.
Despite efforts on the part of the patients to engage in low-calorie diets, some are not able to achieve significant weight loss because of poor compliance with balanced diets and exercise programs. Bariatric surgery, in the form of the jejunoileal bypass, was introduced in 1954 to help patients who were unable to reach weight loss goals on their own and suffered from morbid obesity. Weight loss is achieved by retooling the digestive system to create a malabsorptive state. This procedure was abandoned because it caused significant diarrhea, nutritional deficiencies, and irreversible hepatic cirrhosis in patients. Gastroplasty was first introduced by Gomez 14 in 1981.
In his work, Gomez described stapling the stomach into a smaller gastric pouch that limited the size of meals that could be consumed, thus promoting early satiety. The first gastric bypass was performed in 1967 by Mason and Ito. This procedure combined a small gastric pouch with the bypass of a portion of the small intestine to create a restrictive and malabsorptive means of weight loss. This initial description has been modified over the years to create the Roux-en-Y gas¬tric bypass (RYGB) surgery that has become the mainstay of obesity surgery. For those patients who do not want to undergo a major diversion of their digestive tract, the laparoscopic adjustable band has become a good option. Since its approval by the US Food and Drug Administration in June 2001, many surgeons are using the laparoscopic adjustable gastric band as a means of effecting substantial weight loss without the notable risks associated with open or laparoscopic gastric bypass. More recently, attention has been turned to gastric stapling, which is showing excellent results without many of the complications of gastric bypass, particularly bleeding, anastomotic leaks, adhesive disease, or death.
With the increasing numbers of gastric bypass surgeries being performed, researchers have investigated the high complication rates observed. 17 20 Because of these risks, the physician must have a candid discussion with the patient about risks and benefits of major surgical intervention. In an effort to help patients lose weight without subjecting them to major surgery audits inherent complications, the tongue patch procedure was born.
In this rapid procedure, which has minimal risks and was first introduced in 2009, a mesh prosthesis is placed on the patient’s tongue making it difficult to swallow solid foods. The tongue patch is a means of ensuring that the patient abides by a strict VLCD plan to achieve maximal weight loss while engaging in a moderate exercise regimen (at least 30 minutes of cardiovascular work per day). Applying a mesh prosthesis that makes eating uncomfortable makes it difficult for a patient to continue his or her maladaptive behavior of poor dietary control; the patient is able to regain the upper hand and ideally make long-term lifestyle changes that will lead to weight loss in the short term (treatment period) and successful weight maintenance in the long term. We herein propose a procedure that has minimal risks and the potential to help patients who are obese lose weight, rather than subjecting patients to invasive surgeries that have the potential for significant complications.
Anatomy and Function of the Tongue
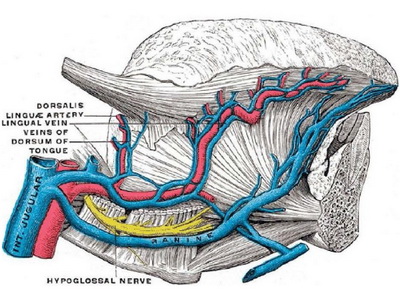
The tongue is the principal organ of taste and is critical in helping propulse food into the oropharynx. Its root is collected to the hyoid bone by the hyoglos sus and genioglossus muscles. The dorsum of the tongue is convex and marked by a medial sulcus, which divides it into symmetrical halves. The musculature of the tongue consists of extrinsic and intrinsic muscles. The extrinsic muscles originate outside the tongue and include the genioglossus, hyoglossus, styloglossus, chondroglossus, and glossopalatinus. In contrast, the intrinsic muscles are contained entirely within the tongue and include the longitudinalis superior and inferior, the transversus, and the verticalis.
The muscles of the tongue are supplied by the hypoglossal nerve. The lingual nerve is a branch of the marginal mandibular nerve (CN V) and supplies sensory innervation to the anterior two-thirds of the tongue. The chorda tympani is a branch of the facial nerve (CN VII) and provides taste to the anterior two-thirds of the tongue. The lingual branch of the glossopharyngeal nerve supplies taste and sensation to the root and sides of the tongue. The main artery of the tongue is the lingual branch of the external carotid. The primary drainage of the tongue is via the lingual vein. These major neurovascular structures are located deep within the tongue along the ventral surface (Figure 1).
During normal swallowing, the tongue undergoes several muscular deformations to move food into the oropharynx. The ingested bolus is initially contained in a groove-like depression in the middle dorsal sur face of the tongue (early accommodation). This depres sion is then translated in a posterior direction until the bolus comes to rest at the posterior edge of the tongue (late accommodation). Finally, the oral stage of the swallow is concluded by the rapid clearance of the bolus retrograde into the oropharynx (propulsion) with a scraping of the bolus along the hard palate and adjustment in the position of the hyoid bone.
Figure 2. Marlex mesh tongue patch in position.
Methods
A retrospective chart review was performed of 81 patients who underwent the tongue patch procedure from 2009 to 2013. Before undergoing the procedure, all patients signed a consent form indicating their understanding that this was an experimental procedure and that the mesh was being used in an off-label fashion to achieve weight loss.
All patients then had a piece of Marlex mesh, the size of a postage stamp, affixed to the tongue. At the 30-day mark, patients were seen to take off the mesh and final weights were recorded. Data were then tabulated for the 69 patients with 30-day data to determine average initial weight and body mass index (BMI), reported comorbidities, and average weight loss over 30 days. Complications were also identified from the patient charts and analyzed.
Procedure in Detail
The patient was brought to the operative suite and placed in the supine position. Before placement of the mesh, the tongue was anesthetized with 4-5 mL of 1% lidocaine with epinephrine to provide local analgesia and vasoconstriction. The Marlex mesh patch was affixed to the tongue using 6 individual 4-0 prolene sutures (Figure 2). After ensuring that patients had no apparent bleeding or observable complications, they were discharged home.
Postoperative Care
Upon discharge from the office, each patient was instructed to return on a weekly basis for weighing, assessment of compliance to the diet and exercise regimen, and counseling. All patients were sent home with a prescription for cephalexin elixir 500 mg 3 times daily for 5 days (if the patient was allergic to penicillin, ciprofioxacin 500 mg twice daily for 5 days was used) and hydrocodone/acetarninophen elixir as needed for pain. Patients were instructed to maintain oral hygiene with an oral mouthwash (eg, Listerine) twice daily with daily brushing and use of dental picks as needed to get rid of matter from below the tongue patch. Patients were also asked to take a multivitamin daily to ensure appropriate supplementation of vita¬mins and minerals. Their source of nutrition was a 250-kcal protein shake providing 19 g protein per meal. These meals were consumed three times daily per physician instruction.
Counseling in the office involved a weekly visit with the patient to discuss their current habits and provide advice on better ways of eating and following a healthy lifestyle. Patients were also given information about a proposed diet of three square meals with two snacks in between for the period after the patch was taken off. The objective is to consume smaller meals spaced throughout the day that are high in fruits and vegetables with small amounts of protein added. If further counseling was necessary, patients were put in touch with a nutritionist on staff at the local medical center who consults for the office. In addition, patients were given the option of communicating with a personal trainer to help establish a reasonable workout routine that takes into account the patient’s needs and limitations while ensuring at least 30 minutes of cardiovascular activity daily (a wide variety of regimens was used and there was no standardization for all patients).
Results*
A total of 81 patients received a tongue patch between 2009 and 2013. Of those patients, only 69 had final weights and heights available for analysis. The mean age of the study population was 39 years (range= 27-51 years). The average starting weight for patients was 188.6lb (range= 161-360 lb). The aver age height for the population was 5 feet 5 inches (range = 5 feet 1 inch to 6 feet tall). The most fre quently reported height (mode) was 5 feet 4 inches. The mean weight loss was 16.0 lb (range= 0-37 lb). The total weight lost by all participants with available 30-day data was 1104.5 lb.
The average starting BMI of patients studied was 32.4 (range = 24.3-45.3). The average BMI at the end of the treatment phase was
29.5 (range = 20.7-41.5). The average change in the BMI was 2.9 (range 0-5.1). Of note, 2 patients failed to lose weight. When patients were further questioned, they admitted to being truant in their diet regimen and exercise progran1s. Although their results were not typical, they were still included in the cohort of 69 completed charts.
Diabetes, hypertension, and hyperlipidemia were the most frequently reported preoperative comorbidities (Table 1). No serious complications noted (Table 2). The most frequent complication was loosening of the patch secondary to stitches falling off (n = 7). This required the patient to return to the office for replacement of the loosened suture. Two patients discontinued therapy prematurely (one at day 10 and the other at day 14) because of difficulty in phonating appropriately.
Although these patients achieved short-term weight loss, they were not able to tolerate the speech difficulty and asked to have the patch taken off. One patient noted pain that lasted beyond the initial expectation of 48 hours of swelling and/or discomfort and phoned the office to notify the physician. She was instructed to take ibuprofen 800 mg 3 times daily, and by her 1-week visit she no longer had any pain or discomfort. No infections, bleeding episodes, or hema tomas were noted during the course of this study.
Although no contact was made with any of the patients’ primary physicians after the treatment period, 3 patients who went on to become surgical patients of the practice said they had been taken off antiliyperten sive medications or the dose had been reduced after having lost weight with the tongue patch.
Table 1. Reported Comorbidities in Patients (N = 81) with a Tongue Patch, 2009-2013
Obesity-Related Comorbidities
- Hypertension
- Hyperlipidemia
- Diabetes
- Osteoarthritis
- Sleep Apnea
No. of Patients
- 42
- 38
- 11
- 10
- 4
% of Patients
- 51.90
- 46.90
- 13.60
- 12.30
- 4.90
Of the 69 patients with complete charts, we were able to communicate with 50 to assess long-term weight loss. Some of the patients were active patients in the practice and could be questioned directly at follow-up visits, and the remainder of the follow-ups were conducted via phone interviews. The follow-ups consisted of simply asking the patients about their satisfaction with the procedure and whether they were able to maintain weight loss after the procedure.
Despite attempts by the authors to encourage long-term changes in lifestyle, dietary habits, and exercise, some patients reverted to their old habits and saw a rebound weight gain. When questioned about their weight gain, many patients cited a love of the “process” of eating.
Of the 50 patients evaluated, 78.0% (39/50) reported that they were happy with the procedure and would recommend it to friends and family. Of the 22% that were dissatisfied, the largest criticism was a lack of long-term support after the patch was taken off, which prevented them from maintaining good lifestyle habits. Another common complaint was the awkward social situation presented by not being able to eat with friends and family during the treat ment phase of the tongue patch diet. Of the 50 patients surveyed, 84% (42/50) maintained their weight loss after the patch was taken off, noting that their success was primarily because they maintained the recommendations provided during the treatment period. The follow-up ranged from 4 months to 3 years and included some of the early patients from 2009.
Table 2. Complications in Patients (N = 81) with a Tongue Patch, 2009-2013
Observed Complications
- Loosening of stitches
- Prolonged Difficulty w/speech
- Pain in the tongue (>48 hrs)
- Infection
- Bleeding
No. of Patients
- 7
- 2
- 1
- 0
- 0
% of Patients
- 8.60
- 2.50
- 1.20
- 0
- 0
Discussion
Over the years physicians have battled the ever increasing obesity problem with various diet regimens and surgical procedures to help those who do not have the willpower to fully help themselves achieve sig nificant weight loss. The tongue patch procedure was designed with the idea of making it uncomfortable to move a bolus of food posteriorly to the oropharynx and hence preventing a patient from cheating on a VLCD. As the tongue contorts during the normal swallowing mechanism, it moves posteriorly and comes into contact with the hard palate. A rough object or hard suture abrading the oral mucosa acts as a deterrent and negative reinforcement for eating foods and helps maintain the patient on a low-calorie liquid diet.
Although the patch does not solve the patient’s long-term issue of establishing appropriate dietary changes and exercise habits, it acts as a pattern interrupt and allows the patient to take the necessary steps to improve dietary habits during the treatment process. Based on the data collected, the tongue patch is useful in patients who are obese (BMI = 30.0-34.9), those who are severely obese (BMI >35) and those who are overweight (BMI = 25.0-29.9).
One patient with a BMI of 24.3 who believed she was overweight was treated and successfully lost weight to achieve a better self image. The wide range of BMis treated points to the fact that the procedure is versatile and can be used to treat a variety of patients. The authors firmly believe that this procedure may even be useful as a weight loss technique before major operations to decrease a patient ‘s preoperative BMI and perioperative morbidity /mortality.
VLCDs like the one used in conjunction with the tongue patch have been the foundation of many weight loss regimens as they significantly cut the consumed calories to no more than 800 kcal per day and allow for rapid and reproducible weight loss. All patients who engage in VLCDs must be under a physician’s care to ensure that they do not experience serious side effects. Many patients on VLCDs report minor reversible side effects, such as fatigue, constipation, nausea, or diarrhea. Patients sometimes complain of arrhythmias secondary to electrolyte imbalances and must be counselled on appropriate vitamin and mineral supplementation to avoid such side effects. The most common serious side effect is gallstones, which can form in patients who are undergoing massive weight loss and have rapid shifts in fluid volumes.
Hydration and constant monitoring by the physician are paramount in this case, and drugs such as ursodiol, which alters bile cholesterol composition and decreases cholesterol synthesis, secretion, and absorption, may be prescribed to prevent their formation. 13 Even with the inherent value of a VLCD, the NIH and National Institute of Diabetes and Digestive and Kidney Diseases agree that obesity treatment requires more than a rapid weight loss, that is, a long-term commitment to long-term changes in healthier eating and regular physical activity.
Various surgical treatments have been proposed to help patients lose weight when they are unable to do so on their own. Particularly in patients who are severely obese, a significant energy deficit must be maintained to produce significant weight loss; it is this fact that pushes many to seek out bariatric procedures that minimize the guess work. Over the decades, the types of surgical procedures used have advanced with the available technology. However, the learning curve has also been quite significant with some of the newer laparoscopic bariatric procedures. Plum and Dellinger, based on administrative data from the state of Washington, reported that surgeons who had performed fewer than 20 procedures had a patient mortality rate of 6% compared with rates near 0% for those who had performed more than 250 procedures. Schauer et al4 reported an anastomotic leak rate of l0% after laparoscopic RYGB in the first 50 procedures and 0% in the subsequent 100 to 150, claiming that there is a 100-case learning curve for performing laparoscopic RYGB.
Suter et al reported on major complication rates during their 2-year experience with laparoscopic RYGB. In their evaluation of 107 cases, they noted a major complication rate of 12.5% in the first two¬ thirds of procedures versus 2.7 % in the last third of procedures performed. These studies show that there is a significant learning curve that must be respected, as it correlates with the complications that can occur. Patients seeking out bariatric surgery should be cognizant of the risks of having the surgery and, more importantly, should only consider having bariatric surgery in centers that specialize in that type of work to avoid higher rates of complication.
As the understanding of the digestive tract has improved and results of various bariatric procedures have been assessed, surgeons have tried to lessen the risks for patients and have sought out surgical techniques that minimize morbidity and mortality from bariatric procedures. Bariatric surgery has moved from jejunoileal bypass in 1954 to laparoscopic gastric stapling procedures in the modern era. However, despite advancements in technology and surgical techniques, bariatric surgeries are not without complications. In a meta-analysis of surgical treatments for obesity, Maggard et al found that the early mortality rate for RYGB was 1.0% in controlled trials and 0.3% for case series data. Adjustable gastric banding had an associated early mortality rate of 0.4% for controlled trials and 0.02% for case series data.
Morbidity associated with bariatric procedures has similarly been evaluated in controlled trials and meta analyses. Nutritional or electrolyte abnormalities have been reported in 17 % of patients undergoing RYGB but also in 3% of patients undergoing vertical banded gastroplasty. Other significant complications observed in various bariatric procedures include respiratory issues (pneumonia, atelectasis, respiratory insufficiency), wound infections (deep and superficial), injury to intra-abdominal organs, hernias (incisional, internal), deep venous thrombosis, pulmonary embolus, anastomotic leaks, and adhesions. In their work for the NIH, Maggard et al 1 looked at the body of literature and found that at a minimum the data suggest that approximately 10% to 20% of patients report adverse events but the occurrence differs among the various procedures.
Without hesitation, one can look at the body of literature and see that surgical intervention for persons who are severely obese (BMI 40) results in greater weight loss than does medical management. Surgical procedures result in 20 to 30 kg of weight loss that is maintained for up to 10 years and longer and is accompanied by significant improvements in several comorbid conditions. For the patients who are obese and have a BMI between 35 and 39, the data also tend to strongly support the superiority of surgical techniques for weight loss. However, that being said, one must always take into account the ever-present potential for complications with surgical intervention.
It is with these risks in mind that physicians have sought less invasive means of helping patients lose weight. In looking back at methods that have been introduced, one must also look at the use of jaw wiring. In the mid 1970’s, jaw wiring became an attractive means of managing patients who were severely obese. The method was largely used because it was believed that patients who were massively obese faced significant operative risks. In addition, jaw wiring was a much more manageable procedure from a cost standpoint.
Patients had their jaws wired shut for anywhere between 6 and 12 months and were placed on a purely liquid diet with multivitamin supplementation. Weight loss was significant in these cases, ranging from 20 to 40 kg. However, many patients noted that weight was rapidly regained after the wires were detached and a regular diet was resumed. In 1981, Garrow and Gardiner went a step further and fastened a nylon cord around the waist of the patient after weight reduction to prevent weight regain. The cord functioned as a psychological barrier against weight gain, which was so common in patients after the jaw wiring was detached. Just as tight clothing might prevent a patient from overeating or prompt the patient to begin dieting, the cord functioned as a means to prevent patients from reverting to old habits that might result in weight gain.
In 2006, Behbehani et al32 evaluated the perceived effectiveness and side effects of intermaxillary fixation and determined that patients had significant weight loss. The results of that study showed that intermaxillary fixation significantly reduced weight by a mean of 6.8 kg during treatment and a mean of 4.1 kg at a minimum of 1 month after it was detached (P < .0001). However, they determined that inter maxillary fixation is not effective for long-term weight reduction and may only be used for a very short period to initiate weight loss. We agree with his conclusions and believe that even the tongue patch is not a long-term solution for patients. This further reinforces the fact that patients must be committed to lifelong lifestyle changes to achieve long-term weight loss; otherwise, they must rely on a crutch of some sort (eg, a cord, tight-fitting clothing) to help them maintain weight loss.
Although the tongue patch works well in helping patients lose weight initially, it does nothing for the patient once detached. Just as Behbehani et al note in their work with intermaxillary fixation, exercise and/or special diet plans are a healthier and better means to treat obesity and maintain weight loss rather than relying on intermaxillary fixation. For that reason, patients are educated on the need for lifestyle changes during the treatment phase of the tongue patch diet, rather than relying on the patch itself as a long-term solution to obesity. Patients who do not make plans for dietary changes and who refuse to engage in regu lar cardiovascular activity are doomed to regain their weight. Just as with other extreme measures to help patients lose weight, failure to change the daily habits that led to obesity in the first place is a recipe for failure.
It is therefore incumbent on the physician to help the patient make long-term changes in eating and exercise habits. The physician-patient relationship is integral to patient success after the tongue patch is taken off. Patients need to feel understood and supported at office visits and should have regular contact with the physician as this has been shown to produce better long-term weight loss maintenance. Weight loss patients may also benefit from visits to a nutritionist or personal trainer to help them during the tongue patch diet or after the patch is taken off, as this will continue to aid in the behavior modification that is so crucial to success.
For this reason, patients who undergo the tongue patch procedure are given the contact information for a certified nutritionist and certified personal trainer associated with our facility should they require further assistance in reaching their weight loss goals before or after treatment. In addition, to help ensure post-procedural success, patients are given a sample diet plan to follow. This diet plan relies heavily on small portions and is primarily plant and vegetable based with small amounts of protein added to maintain a healthy and balanced diet.
This study has several limitations. The first is the retrospective nature of this study. A more powerful study would be one performed prospectively. Second, some patients were lost to follow-up, making the power of the study significantly diminished as there was incomplete data for 12 study participants. Third, there was no control arm for this study to determine if it was in fact the use of the tongue patch and the VLCD that produced the effects for these patients. Therefore, calculation of statistical significance cannot be appropriately performed. Thus, we will be developing a prospective study of the use of tongue patch versus simple diet and exercise. Fourth, there was no long-term assessment of success with the tongue patch. Although it was clearly impressed on all patients that long-term lifestyle and dietary changes were a must, it is unclear if all patients adhered to these instructions and maintained their weight loss after the patch was taken off. Our study demonstrated a retained weight loss in 84% of our patients; however, it would be interesting to assess weight loss maintenance closer to 5 years from initial treatment period. Also, it would be more helpful to follow patients prospectively to truly evaluate the overall success of the treatment.
Finally, although satisfaction was evaluated it would be helpful to perform patient assessments prospectively during the course of their treatment, having them cite specific areas of the treatment program that were helpful or not helpful in providing a successful result. In future evaluations of the procedure, having patients complete a standardized questionnaire at regular intervals would be helpful in assessing not only success of the procedure but also patient satisfaction.
Conclusion
Surgical intervention for patients who are severely obese is effective in achieving long-term weight loss with reduction in associated comorbidities; however, this comes with a risk of postoperative morbidity and mortality. For patient’s concerned with the risks of sur gery, less invasive methods of weight loss should be considered. Although less invasive techniques rely on patient compliance and willingness to make long-term lifestyle changes, they may be an option in appro priately selected patients. This study demonstrates that patients can achieve significant weight loss in a 30- day period with relatively minimal procedural risk while maintaining a strict low calorie diet with the assistance of the tongue patch and adhering to a regular exercise regimen.
*INDIVIDUAL RESULTS WILL VARY. TESTIMONIALS DO NOT CONSTITUTE A PROMISE OR REPRESENTATION OF ANY PARTICULAR OUTCOME OR EXPERIENCE.